Temps de lecture : 5 min
3 décembre 2024
SANTÉ COMMUNAUTAIRE ET MONDIALE
Histoire impactante
Strides Toward Early Infant Diagnosis for HIV Elimination in South Africa
Landiwe, a young South African mother, was diagnosed with human immunodeficiency virus (HIV) in 2017 while she was pregnant. Her baby was born HIV-positive, putting her tender life at risk.
Each year globally, an estimated 1,3 million women and girls living with HIV become pregnant.1 Without intervention, the rate of transmission from HIV-positive mothers to their babies during pregnancy, labor, delivery, or breastfeeding (vertical transmission) is 15-45%.1
Globally, 1,5 million children (0-14 years) were living with HIV in 2022.2 This is a small proportion of the 39 million total people living with HIV,2 but infants and children suffer worse outcomes because their immune systems are not fully developed. Thus, prevention, testing, and treatment are essential.
Progress in Preventing Mother-to-Infant Transmission
Huge advances in testing and treatment have been made in recent decades, leading to vertical transmission rates below 5% in many countries, including Ethiopia, South Africa, and Tanzania, and the elimination of vertical transmission in many others, including Armenia, Belarus, the Caribbean, Cuba, and Thailand.3
The 2023 UNAIDS Global AIDS update noted steep drops in the number of new infections among children due to effective interventions.4 AIDS-related deaths among children were reduced by 64% in 2010–2022,4 and programs to avoid vertical transmission prevented 3,4 million new HIV infections in children since 2000.5 These are encouraging developments in the fight against AIDS. Still, the HIV pandemic claimed the lives of approximately 84 000 children in 2022.4 This is still too many.
Advances in Vertical Transmission Herald New Challenges
Dr. Philip Goulder, a renowned pediatric HIV researcher and Professor of Immunology at Oxford University, agrees that mother-to-baby transmission has been decreasing thanks to advances in healthcare and treatment. He explains that as a result, babies' viral loads at birth are sometimes very low, and without immediate, sensitive testing at the point of care, they can be lost to follow-up, meaning they miss out on life-saving treatment. Dr. Goulder notes that, “if they manage to survive, several months later, they have huge viral loads, and their immune systems are damaged irrevocably.”
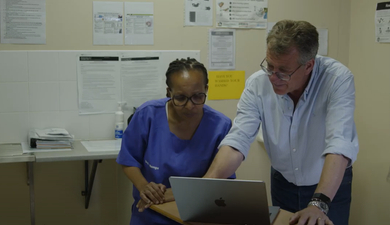
The same trend was observed by Dr. Nomonde Bengu, a clinician who cares for mothers and babies at the Queen Nandi Regional Hospital in South Africa. Dr. Bengu notes that “there was a concern about the rising number of positive infants at their 10-week review.” She highlights the challenge in these cases: “The question becomes whether it was a missed positive at birth because of potent antiretroviral therapy or postpartum transmission. To discern this, we think point-of-care testing would assist.”
Solutions to Identify HIV-Positive Babies Early
Dr. Goulder started a ‘Baby Cure’ study in KwaZulu-Natal, South Africa, in 2015 with the goal of further understanding HIV and the potential for HIV cure in children. Under this program, babies who are HIV-infected in utero are diagnosed using point-of-care testing at birth, and antiretroviral therapy is initiated within hours.
Dr. Bengu and her team have partnered with Dr. Goulder in this much-needed work to bring sensitive HIV testing to patients as early as possible. Dr. Bengu notes that mothers worry less once they know what they’re facing and that they can start treatment right away.
Source : https://www.youtube.com/watch?v=WA_ad0Klzus
It was through the Baby Cure study that Landiwe’s HIV status was identified in 2017. Thanks to onsite point-of-care testing, her baby daughter’s status was also identified, and she started therapy immediately. With early diagnosis and therapy initiation, along with access to ongoing care, Landiwe’s daughter is an HIV success story. She celebrated her 6th birthday in 2023 with other survivors, healthcare workers, and well-wishers at the Queen Nandi Hospital.

Source : https://www.youtube.com/watch?v=WA_ad0Klzus
Toward HIV Eradication in Children
The World Health Organization (WHO) recommends point-of-care nucleic acid (e.g., PCR) testing to diagnose HIV among infants and children younger than 18 months of age.6 The WHO recently granted prequalification status to Cepheid’s Xpert HIV-1 Qual XC test, an improved PCR test to detect HIV-1 in infants, adolescents, and adults. “WHO prequalification aims to ensure access to key health products that meet global standards of quality, safety and efficacy/performance, in order to optimize use of health resources and improve health outcomes.”7
To meet the global need for timely HIV testing outside of traditional healthcare settings, the Xpert HIV-1 Qual XC test was designed for use in laboratories and at the point of care, enabling same-day results. The Baby Cure team used an earlier version of this test to provide point-of-care results for Landiwe and many others. This test adds a tool to the global community’s ongoing efforts to eradicate infant HIV so all children can live full and healthy lives.
Watch Dr. Bengu discuss the Baby Cure Trial at Queen Nandi Regional Hospital Empange, South Africa:
Londiwe Thungo: My name is Londiwe Thungo from Ndlangubo. I’m 35 years old. I've been coming to the Queen Nandi Regional Hospital since delivering my daughter, Anotha Mthembu in 2017. I was diagnosed with HIV in 2017 when I was pregnant.
Ncamisile Mazibuko: My name is Ncamisile Mazibuko and I am here with my child, Amile Minenhle Ntuli. I tested in 2018 and the results were positive.
Dr. Nomonde Bengu: “Our hospital has been involved in a study called the Baby Cure trial where we were screening high-risk mothers with HIV with our point of care testing and identifying the positive babies and initiating ART right away.
Dr. Philip Goulder: “The mother-to-child transmission rates have fallen massively since the last 20 years but as they become lower and lower below one percent in the case of in utero infection, the viral loads of the level of virus in the infected babies is really really low so you actually need to have a point of care test in many cases to make the diagnosis.
An issue with not making a diagnosis is that these kids essentially lost to follow-up and when we pick them up some months later if they've survived, they will have huge viral loads, and their immune systems will be you know damaged irrevocably so for us it's really massively important to have the point-of-care testing that we're doing now.
Londiwe Thungo: My result came back immediately so they told me my baby was HIV positive but I saw other children they lived their lives if they took their medication and so my baby started to take medication.
Ncamisile Mazibuko: “It was painful when I discovered that my child is positive, I received counseling from the Doctor, and I knew I was not alone in the journey.
Dr. Nomonde Bengu: I find that the mothers, they worry less, and because they know once they leave the hospital, they know exactly what they're facing and they go home and start treatment right away.
Dr. Philip Goulder: “The opportunity that one has in studying mothers and children is right here to make the diagnosis you need to have your point of care testing done right at as early as possible and then you're maximizing your chances of achieving a cure in those kids.”
CE-IVD. Dispositif médical de diagnostic in vitro. Les tests ne sont pas tous disponibles dans tous les pays.
Références :
1. WHO. Mother-to-child transmission of HIV https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/hiv/prevention/mother-to-child-transmission-of-hiv. Consulté le 2/29/2024
2. UNAIDS Gloabl HIV & AIDS statistics – Fact Sheet https://www.unaids.org/en/resources/fact-sheet accessed 2/29/2024
3. Vrazo AC, Sullivan D, Phelps R. Eliminating mother-to-child transmission of HIV by 2030: 5 strategies to ensure continued Progress. Glob Heal Sci Pract. 2018;6(2):249–56. doi: 10.9745/GHSP-D-17-00097 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6024627/
4. UNAIDS Global AIDS Update 2023. https://thepath.unaids.org/#:~:text=This%20report%20makes%20clear%20that,clear%20what%20that%20path%20is. Consulté le 2/29/2024
5. The U.S. President’s Emergency Plan for AIDS Relief (PEPFAR). San Francisco, CA: Kaiser Family Foundation; 2023 https://www.kff.org/global-health-policy/fact-sheet/the-u-s-presidents-emergency-plan-for-aids-relief-pepfar/. Accessed 2/29/2024
6. World Health Organization. (2021). Guidelines: updated recommendations on HIV prevention, infant diagnosis, antiretroviral initiation and monitoring. World Health Organization. https://www.who.int/publications/i/item/9789240022232. Consulté le 3/21/2024
7. WHO Prequalification: Impact on Global Access. Presented by Deus Mubangizi, Unit Head, Prequalification Unit, Regulation and Prequalification, WHO. https://www.fda.gov/media/166136/download#:~:text=%E2%80%A2%20WHO%20prequalification%20aims%20to,resources%20and%20improve%20health%20outcomes. Consulté le 2/29/2024